La salute digitale è un’area di indagine in crescita e in evoluzione. Recenti studi hanno valutato l’impatto dell’uso delle tecnologie sanitarie digitali per migliorare i risultati delle CVD attraverso diverse modalità: programmi di messaggistica testuale, applicazioni per smartphone (app) e dispositivi indossabili. I programmi di messaggistica testuale sono ad oggi il tipo di intervento sanitario digitale più studiato; è stato dimostrato che favoriscono una riduzione del rischio di CVD e una migliore aderenza ai farmaci. Anche la letteratura a sostegno dell’uso delle app per smartphone è in crescita, ma rimane limitata, con alcuni studi che favoriscono l’uso di app per la salute ma altri che mostrano risultati negativi. I dispositivi indossabili, invece, sono l’ultimo tipo di tecnologia studiata, ma l’evidenza scientifica ne ha mostrato risultati sempre positivi in termini di attività fisica e rilevamento delle aritmie.
Le malattie cardiovascolari sono la principale causa di morte a livello globale. Nel 2016, l’Academic Research Organization, Hospital Israelita Albert Einstein di São Paulo, ha stimato a circa 470 milioni la prevalenza globale delle CVD e ha registrato circa 17,6 milioni di decessi a causa delle CVD in tutto il mondo. Inoltre, il numero di decessi dovuti a CVD è aumentato di circa il 15% tra il 2006 e il 2016, e questo aumento è dovuto principalmente a un aumento dei decessi dovuti a cardiopatia ischemica. È importante sottolineare che oltre i tre quarti di questi decessi si sono verificati nei paesi a basso e medio reddito, dove i tassi di mortalità cardiovascolare sono sostanzialmente superiori a quelli dei paesi ad alto reddito.
Il termine CVD comprende una vasta gamma di malattie, comprese le cardiopatie ischemiche, le malattie cerebrovascolari, le cardiopatie ipertensive, le malattie cardiovascolari periferiche, le cardiopatie reumatiche, le cardiomiopatie e le aritmie. La maggior parte delle CVD è correlata a una combinazione di fattori di rischio comportamentali e metabolici. Importanti fattori di rischio comportamentali modificabili includono il fumo, l’inattività fisica e una dieta malsana. La presenza a lungo termine di fattori di rischio comportamentali può portare a fattori di rischio metabolico, come ipertensione, il diabete, la dislipidemia e sovrappeso/obesità. Questo per dire che il fulcro della gestione e della prevenzione delle CVD si basa su interventi per motivare la modifica dello stile di vita e l’aderenza a farmaci cardiovascolari efficaci. Strategie efficaci per promuovere l’eliminazione del vizio del fumo, per aumentare i livelli di attività fisica, per motivare a seguire una dieta sana e migliorare l’efficacia dei farmaci sono associate a miglioramenti della morbilità e alla riduzione della mortalità. Tuttavia, dato il numero di persone a rischio per o con CVD, ci sono sfide pratiche, logistiche, geografiche e finanziarie associate alla fornitura di una gestione completa dei fattori di rischio a diverse popolazioni. I sistemi sanitari di tutto il mondo sono incaricati di trovare modi per raggiungere più persone in modo efficiente e scalabile.
Focus sulla Digital Health
Il termine Digital Health indica l’utilizzo di tecnologie digitali, mobili e wireless a sostegno del conseguimento degli obiettivi in materia di salute. Recentemente, il termine salute digitale è usato sempre più spesso per descrivere l’uso delle tecnologie dell’informazione e della comunicazione per la salute, e comprende gli interventi di eHealth e mHealth, nonché settori emergenti come l’analisi dei big data, l’intelligenza artificiale (AI) e l’apprendimento automatico.
Le tecnologie sanitarie digitali stanno trasformando l’assistenza sanitaria facilitando la prevenzione, la diagnosi e la gestione delle malattie, consentendo a pazienti e operatori sanitari di ottenere risultati sanitari migliori.
In una risoluzione pubblicata nel 2018, l’Organizzazione Mondiale della Sanità (OMS) ha esortato le organizzazioni sanitarie di tutto il mondo a dare priorità allo sviluppo, alla valutazione, all’attuazione e all’espansione delle tecnologie sanitarie digitali e a integrare queste nuove tecnologie nelle infrastrutture dei sistemi sanitari esistenti. Come affermato dal direttore generale dell’OMS in un’altra relazione pubblicata nel 2019, la sanità digitale ha il potenziale per colmare il divario tra le disuguaglianze in materia di accesso alla salute, migliorando la portata e rafforzando i sistemi sanitari. Il potenziale degli interventi sanitari digitali è diventato ancora più rilevante durante la pandemia da COVID-19, in cui l’isolamento sociale ha aumentato la necessità di una rapida proliferazione della medicina digitale e ha portato alla luce alcune delle restrizioni normative che rendono difficile l’espansione digitale.
La salute digitale è un settore dinamico e in continua evoluzione che richiede nuovi approcci per valutare l’efficacia e l’efficienza di queste tecnologie innovative. Per rispondere a questa esigenza, l’OMS ha pubblicato una guida su come monitorare e valutare le tecnologie sanitarie digitali. In questa guida vengono presentate diverse raccomandazioni, tra cui le modalità di selezione del disegno dello studio e degli indicatori per valutare al meglio un intervento sanitario digitale, i componenti e gli strumenti chiave per il monitoraggio sanitario digitale, i diversi approcci alla valutazione della qualità dei dati e le linee guida per la segnalazione dei risultati – in particolare la checklist mHealth Evidence Reporting and Assessment (Mera). La guida sottolinea anche l’importanza di includere metodi quantitativi ed economici nella valutazione degli interventi sanitari digitali. Inoltre, anche la Food and Drug Administration (FDA) degli Stati Uniti sta rimodellando la propria supervisione e regolamentazione sulle tecnologie digitali per la salute, riconoscendo che l’approccio basato sul rischio è necessario per regolamentare adeguatamente le tecnologie sanitarie digitali, pur continuando a promuovere l’innovazione. Uno dei nuovi approcci della FDA alla supervisione della salute digitale è stata la creazione del Digital Health Program, in cui sono state create diverse politiche per consentire la lettura di tecnologie a basso rischio a disposizione del pubblico, assicurando al contempo che queste tecnologie digitali siano di alta qualità, sicure ed efficaci. Mentre gli interventi sanitari digitali hanno il potenziale per un impatto significativo e su larga scala sull’assistenza sanitaria, l’attuazione di tali interventi deve essere effettuata con un’attenta valutazione delle prove scientifiche dei rischi e dei benefici di tali interventi, in modo da non sprecare risorse in interventi inefficaci.
Interventi sanitari digitali per migliorare la cura CVD
Per quanto riguarda le CVD, le applicazioni delle tecnologie sanitarie digitali sono potenzialmente numerose. Ad esempio, per scopi diagnostici, un trasduttore di un ecocardiogramma collegato a uno smartphone o un tablet può essere utile per la diagnosi di cardiopatia valvolare in situazioni di reddito a risorse limitate laddove una macchina per ecocardiogramma standard non è ad esempio disponibile. Inoltre, i dispositivi indossabili, come gli smartwatch, possono aiutare la diagnosi di aritmie che richiedono il monitoraggio continuo del ritmo, dove lunghi periodi di monitoraggio in precedenza sarebbero stati fattibili solo con l’impianto di un registratore di loop. Attraverso polsini collegati a un’app per smartphone tramite Bluetooth si facilita il monitoraggio della pressione sanguigna da casa utile a guidare il trattamento. Ai fini del trattamento, la stampa 3D potrebbe essere utilizzata come potenziale soluzione per produrre valvole cardiache a basso costo per la sostituzione delle valvole in futuro. Inoltre, l’AI può essere utilizzata per assistere lo sviluppo di nuovi farmaci e l’apprendimento automatico per prevedere i risultati CVD. Sebbene la salute digitale abbia un enorme potenziale per migliorare la prevenzione e l’assistenza alle malattie cardiovascolari, ad oggi vi sono poche prove scientifiche a sostegno dell’uso delle tecnologie sanitarie digitali. Le principali sfide che stanno ancora ostacolando l’adozione diffusa di tecnologie indossabili intelligenti nella pratica clinica riguardano l’accuratezza dei dispositivi, la validità clinica, la mancanza di politiche normative standardizzate e le preoccupazioni per la privacy dei pazienti, ma un’integrazione metodica degli smart wearable devices nel flusso di lavoro clinico per una cura ottimale del paziente non solo è possibile, ma anche potenzialmente rivoluzionaria.
In questa sezione, esamineremo tre principali tipi di interventi che sono stati più studiati fino ad oggi e sono supportati da rigorosi studi clinici ben condotti:
- programmi di messaggistica di testo
- applicazioni per smartphone (app)
- dispositivo indossabile
I programmi di messaggistica testuale
I programmi di messaggistica testuale sono il tipo di intervento sanitario più studiato, essendo una tecnologia relativamente vecchia dei primi anni 2000. Fin dal l’inizio del loro utilizzo, i messaggi di testo sono diventati un mezzo di comunicazione comodo, frequente e poco costoso che non richiedeva la connessione a Internet. Nel settore sanitario, i messaggi di testo sono diventati anche uno strumento attraente per la comunicazione con i pazienti, poiché i messaggi di testo possono essere inviati a un gran numero di persone contemporaneamente con un input umano minimo attraverso un software automatizzato, possono essere acquistati all’ingrosso riducendo il costo per il provider ed è solitamente percepito come un modo non intrusivo di comunicazione. Inoltre, gli interventi trasmessi tramite messaggi di testo possono raggiungere persone che hanno un accesso limitato all’assistenza sanitaria, come quelle che vivono in aree rurali e remote. Nel contesto delle CVD, i messaggi di testo sono stati utilizzati per migliorare due aspetti fondamentali della gestione delle malattie: i comportamenti di stile di vita e l’aderenza ai farmaci. L’eliminazione del fumo è stato uno dei primi comportamenti di vita ad essere pubblicizzato tramite programmi di messaggistica. Diversi studi hanno avuto lo scopo di valutare se i messaggi di testo potessero migliorare la sospensione del fumo e ne hanno dimostrato l’efficacia. Alla luce di questi risultati, i governi e le organizzazioni mediche offrono ora programmi di messaggistica di testo gratuiti per sostenere coloro che desiderano smettere di fumare, come il programma SmokefreeTXT negli Stati Uniti e il programma Short Messages against Tobacco (SMAT) in Canada. L’inattività fisica è un altro comportamento dello stile di vita studiato in molti studi di messaggistica testuale. Revisioni sistematiche pubblicate di recente hanno valutato se i programmi di messaggistica testuale fossero efficaci nel promuovere l’attività fisica e hanno dimostrato ad esempio la registrazione di un aumento significativo del numero di passi al giorno e i benefici dei programmi di messaggistica di testo sulla perdita di peso nei partecipanti in sovrappeso e sull’aderenza dei farmaci nei pazienti affetti da una varietà di condizioni croniche.
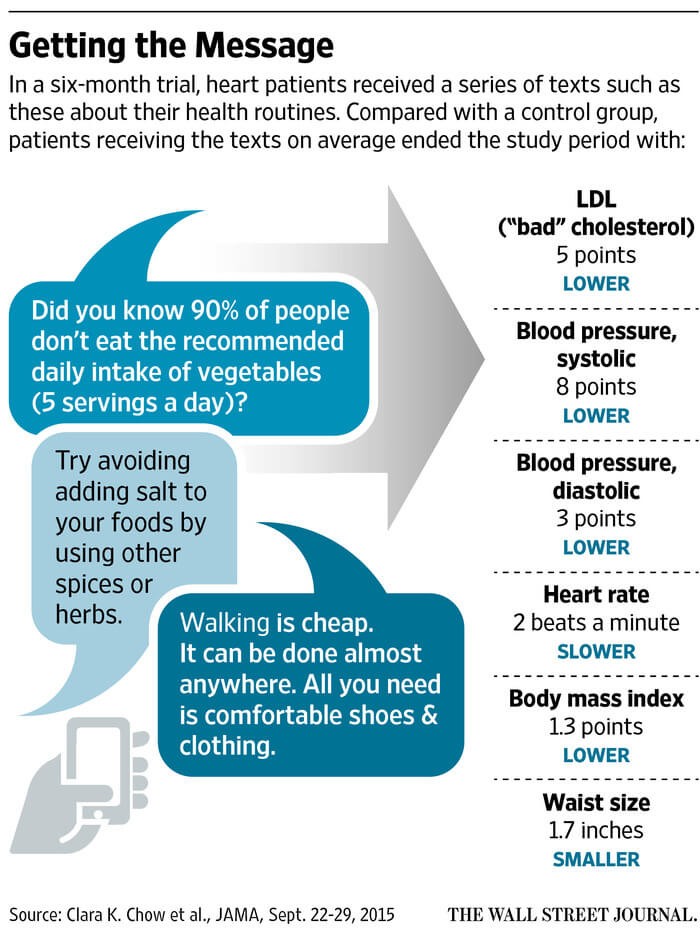
Per chi volesse approfondire, particolarmente importante è lo studio TEXT ME, pubblicato nel 2015, uno dei pochi RCT robusti pubblicati fino ad oggi che ha studiato gli effetti dei messaggi di testo su molteplici comportamenti sanitari.
Smartphone Apps
Con l’avvento di smartphone e tablet, gli interventi di salute digitale forniti tramite questi nuovi dispositivi hanno iniziato a crescere in modo esponenziale. Interventi forniti tramite smartphone e tablet sono di interventi di messaggi di testo più sofisticati, in quanto questi dispositivi più recenti sono in grado di eseguire applicazioni, ovvero programmi simili al computer con molte funzionalità. Le app possono educare i pazienti attraverso informazioni scritte e visive e monitorare e gestire le condizioni di salute attraverso diari e promemoria automatici integrati. Anche se c’è un enorme potenziale per le applicazioni di salute, c’è un aspetto importante da considerare: a differenza dei programmi di messaggistica testuale, le app per la salute sono spesso sviluppate con pochi o nessun input da parte dei professionisti della salute e non sono guidate da linee guida basate su prove. Centinaia di migliaia di applicazioni per la salute sono messe a disposizione del pubblico negli app store, ma ciò avviene con poca investigazione sul fatto che tali applicazioni siano benefiche o dannose per i pazienti. Date le numerose funzionalità potenziali di un’app per la salute, è importante creare un’app che si concentri sulle funzionalità in grado di influenzare il comportamento di un individuo. Nel 2015 è stata pubblicata un’interessante rivista sull’evoluzione delle applicazioni per smartphone nella prevenzione CVD. Gli autori discutono che le app di prevenzione CVD dovrebbero avere alcuni componenti fondamentali per promuovere il cambiamento del comportamento. Concludono che queste app in definitiva dovrebbero:
- essere semplici
- avere informazioni credibili
- basarsi su concetti di cambiamento comportamentale
- utilizzare il monitoraggio dei dati in tempo reale per monitorare i comportamenti
- fornire ricompense per motivare i pazienti a tenere il passo
- avere informazioni personalizzate
- avere elementi sociali per coinvolgere i pazienti
- garantire la privacy
Una recente revisione sistematica pubblicata nel 2018 aveva lo scopo di valutare l’efficacia, l’accettabilità e l’utilità delle app sanitarie per la gestione e il controllo dei CVD. Gli autori hanno esaminato la letteratura pubblicata fino ad aprile 2017 e hanno trovato 10 studi con un totale di 607 pazienti. Gli interventi sono stati vari e mirati a diverse popolazioni di pazienti con ipertensione, cardiopatia coronarica, insufficienza cardiaca e ictus. Solo tre studi erano RCT e, a causa dell’eterogeneità degli studi, non è stata effettuata una meta-analisi.
- Lo studio di Morawski et al. pubblicato nel 2018 mirava a valutare se un’app per smartphone migliorasse l’aderenza ai farmaci e il controllo della BP nei pazienti con ipertensione incontrollata.
- Lo studio pubblicato da Santo et al. nel 2019 mirava a valutare se le app di promemoria dei farmaci migliorassero l’aderenza ai farmaci e altri risultati clinici, come i livelli di BP e colesterolo
- Lo studio di Redfern et al. ha valutato se una strategia di salute digitale diretta dal consumatore per la gestione del rischio di CVD – che comprendeva un sito web e un’app di accompagnamento (CONNECT) – migliorerebbe l’aderenza ai farmaci e i risultati clinici in pazienti con rischio moderato o elevato di CVD
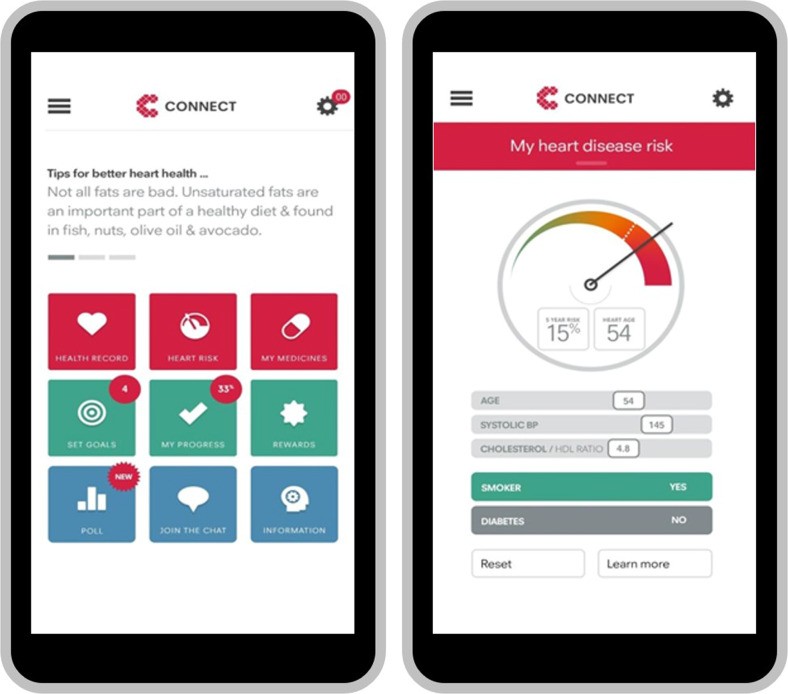
I risultati hanno mostrato che gli utenti di app hanno avuto miglioramenti in termini di BP, BMI, circonferenza vita, colesterolo, attività fisica, aderenza dei farmaci, tassi di ricovero, conoscenze specifiche sulla malattia, benessere psicofisico, hanno smesso di fumare e hanno migliorato la qualità della vita. Questa recensione ha anche valutato le caratteristiche delle app e ha trovato che le caratteristiche delle app accattivanti comprendevano il monitoraggio dei comportamenti sanitari, l’auto-monitoraggio, le informazioni sulle malattie e i contenuti personalizzati/personalizzabili. Anche se i risultati indicano un potenziale beneficio di applicazioni sanitarie per la cura CVD, gli autori avvertono che la bassa qualità delle prove fino ad oggi – dato il piccolo numero di RCT, le piccole dimensioni del campione e la breve durata degli interventi – limiti l’interpretazione di questi risultati.
Wearable devices
I dispositivi indossabili sono dispositivi elettronici che possono essere indossati e hanno la capacità di acquisire informazioni, eseguire elaborazioni dati e fornire l’output delle informazioni pertinenti tipicamente tramite una connessione con un altro dispositivo, ad esempio un’app per smartphone. Date queste caratteristiche, i dispositivi indossabili sono diventati sempre più popolari nelle impostazioni sanitarie in quanto possono essere utilizzati come strumenti per monitorare in tempo reale e continuamente dati come segni vitali, attività e comportamenti. Queste informazioni pertinenti fornite dai dispositivi indossabili possono, a loro volta, aiutare i professionisti della salute a prendere decisioni cliniche informate. Nel contesto della cura e della gestione CVD, il primo fattore di stile di vita che viene preso in considerazione è l’attività fisica. I tracker di attività basati sui consumatori, come Fitbit, sono ora ampiamente disponibili nei negozi di tutto il mondo con prezzi accessibili. Questi activity tracker forniscono informazioni sul conteggio dei passi, sulla distanza percorsa, sul dispendio energetico e sulla frequenza cardiaca. Quando sono collegati alle app per smartphone, i tracker di attività possono essere strumenti motivazionali, che ricordano agli individui di essere fisicamente attivi, fornendo ricompense virtuali quando si raggiunge un obiettivo e offrendo supporto tra pari condividendo i risultati delle prestazioni per stimolare un ambiente simile alla concorrenza. Data l’ampia disponibilità e la crescente popolarità di questi tracker di attività, molti studi hanno valutato se l’uso di tali dispositivi può migliorare i livelli di attività fisica.
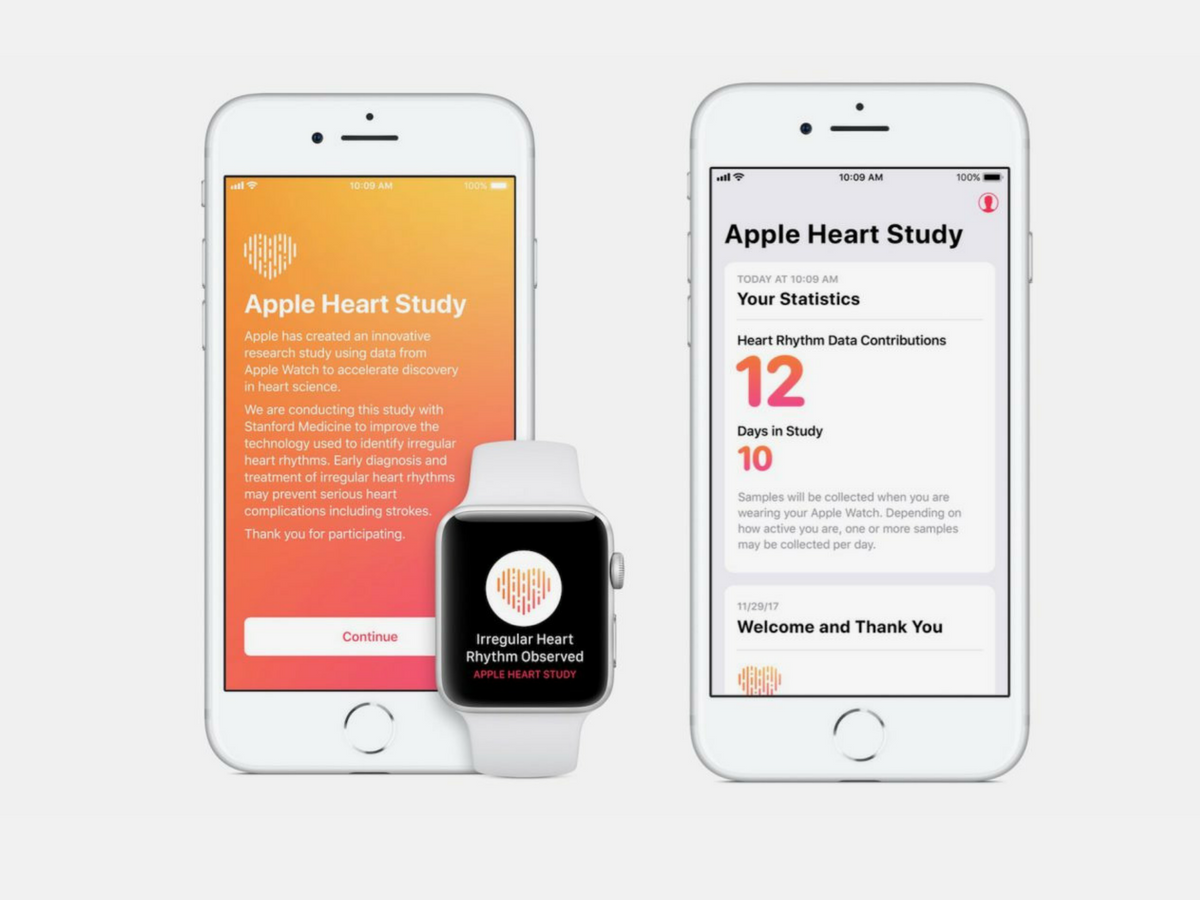
L’Apple Heart Study è stato uno studio innovativo, pubblicato nel 2019, che mirava a valutare la capacità di un algoritmo di notifica del polso irregolare di rilevare la fibrillazione atriale (AF) con l’uso di uno smartwatch, l’Apple Watch. Lo studio era un intero studio pragmatico virtuale, in cui i potenziali partecipanti erano individui che possedevano un Apple Watch e un iPhone compatibile, di 22 anni o più, che risiedevano negli Stati Uniti, parlavano inglese, che non avevano alcuna storia precedente di AF e che in quel momento non stavano prendendo anti-coagulanti. I potenziali partecipanti hanno dovuto caricare l’app di studio nell’app store per verificare l’idoneità e fornire il consenso informato prima che la notifica dell’impulso irregolare fosse attivata sullo smartwatch. Al momento dell’attivazione, l’algoritmo dell’app iniziava a valutare il ritmo cardiaco utilizzando il sensore fotopletismografico dello smartwatch – che utilizza luci a LED per misurare in modo intermittente i cambiamenti nel flusso sanguigno. Questi segnali di impulso sono stati usati per generare un grafico di intervallo di impulso (tacogramma) che allora è stato classificato come regolare o irregolare. Un partecipante riceveva una notifica irregolare del polso se 5 tachigrafi su 6 fossero stati considerati irregolari in 48 ore. Se il partecipante riceveva questa notifica irregolare del polso, aveva in programma una consultazione di telemedicina con un medico che avrebbe valutato se il caso richiedesse un’ulteriore valutazione. In caso affermativo, ai partecipanti sono stati spediti una patch ECG da indossare per un massimo di 7 giorni per confermare l’aritmia. Sulla base dei risultati gli autori hanno riferito che il valore predittivo positivo di un singolo tachigrafo irregolare era 0,71 (95% CI 0,69-0,74), il che significa che il 71% del tempo in cui un tachigrafo ha rilevato un impulso irregolare, l’AF è stata rilevata anche dalla patch ECG. Nel frattempo, il valore predittivo positivo della notifica di impulsi irregolari era 0,84 (95% CI 0,76-0,92), il che significa che l’84% delle volte in cui un partecipante ha ricevuto una notifica di impulsi irregolare, il partecipante ha ricevuto una notifica irregolare del polso, il partecipante ha confermato l’AF sull’ECG simultaneo.
Conclusione
La salute digitale è un’area di indagine in crescita e in evoluzione. Ad oggi, i programmi di messaggistica testuale sono il tipo di interventi sanitari digitali più supportati da prove scientifiche con studi che mostrano potenziali benefici per la cessazione del fumo, l’attività fisica, la pressione sanguigna e il controllo del colesterolo, gestione del peso e l’aderenza ai farmaci. La letteratura per supportare l’uso di app per smartphone nella prevenzione CVD è in crescita, ma è ancora limitata ma piccoli studi hanno favorito l’uso di app per la salute per migliorare i risultati sanitari del CVD. I dispositivi indossabili sono l’ultimo tipo di tecnologia investito negli studi clinici. Gli studi supportano l’uso di tracker di attività fisica per migliorare i livelli di attività fisica, mentre gli smartwatch possono essere utilizzati come un nuovo strumento per rilevare aritmie.
È importante sottolineare che la tecnologia digitale ha il potenziale per superare diverse barriere, come la geografia e il tempo, e quindi, anche con risultati sanitari equivalenti alle cure standard, ci sono enormi aspetti positivi in termini di portata dal punto di vista della salute pubblica. Inoltre, gli interventi sanitari digitali non dovrebbero essere visti come una soluzione a sé stante e unica per tutti, ma piuttosto come un’aggiunta agli attuali interventi sanitari multifase che possono essere personalizzati per diversi tipi di popolazioni di pazienti. Possiamo considerare questi strumenti come un modo per ottenere migliori risultati per la salute dei pazienti, ma anche come modi innovativi per reinventare il modo in cui attualmente vengono condotti studi clinici. Queste tecnologie digitali possono consentire nuovi modelli di prove virtuali, riducendo potenzialmente la durata e i costi della ricerca futura, aumentando nel contempo la capacità di ottenere risultati significativi.
Source: Digital Health Innovations to Improve Cardiovascular Disease Care Karla Santo1,2,3 & Julie Redfern2,3 |10 September 2020 / Published online: 3 October 2020 | Springer Science+Business Media, LLC, part of Springer Nature 2020
